Abstract
Background:
Von Willebrand Disease (VWD) is the most common inherited bleeding disorder in the United States. Despite von Willebrand factor (VWF) antigen and activity levels rising during pregnancy particularly in those with type 1 disease, there are several obstetric concerns regarding patients with VWD, including epidural management, mode of delivery, fetal outcome, and postpartum hemorrhage. Current guidelines suggest achieving a VWF activity (RCoF) and factor VIII:C level of at least 50 IU/dL before delivery, with maintenance > 50% of normal for at least 3-5 days.
Aim:
To investigate the incidence of obstetric complications in women with VWD and correlate maternal and fetal outcomes with VWF levels.
Methods:
We conducted a single-institution retrospective observational study reviewing the charts of all women diagnosed with VWD at the Hemophilia Treatment Center from January 2000 to June 2017. We included women with single or multiple pregnancies. We assessed the following obstetric outcomes: bleeding episodes during pregnancy, mode of delivery, use of epidural anesthesia, perioperative management of bleeding, prophylactic measures during peripartum period, presence of postpartum hemorrhage or excessive incisional bleeding, rate of spontaneous fetal loss, VWF/VIII:C levels during perioperative period, and transfusions. We excluded women with other diagnosed bleeding disorders. Statistical analyses were performed using the unpaired Student's t test.
Results:
The charts of 231 females with VWD were reviewed. There were 71 total pregnancies from 46 patients that were evaluable. 93.5% (43/46) patients had Type 1 VWD. 9.9% (7/71) had bleeding prior to delivery which included ecchymoses, mucosal or gingival bleeding, vaginal spotting, or epistaxis. Regional epidural anesthesia was performed in 16.9% (12/71) of cases with no bleeding complications reported. 25.4% had documented C-sections and 60.6% had vaginal deliveries. Postpartum bleeding (defined as immediate or delayed excessive vaginal or incisional bleeding) occurred in 29.6% (21/71) of cases; 38.9% (7/18) who underwent C-section and 25.6% (11/43) in vaginal deliveries. 50% (6/12) developed heavy bleeding despite receiving preoperative desmopressin (DDAVP) or human factor VIII/human VWF complex. 61.9% (13/21) required transfusions of blood products (either packed red blood cells or platelets), surgical dilation and curettage, IV/IN DDAVP or FVIII/VWF concentrates. 7% (5/71) had complications which included two ectopic pregnancies, two miscarriages, and one stillbirth, and one of these resulted in postpartum heavy bleeding (20%).
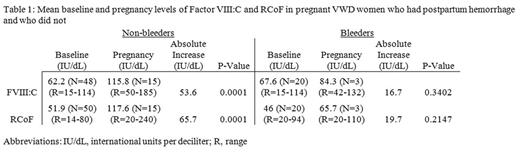
The baseline and third trimester factor VIII:C and RCoF levels of non-bleeders and bleeders are shown in Table 1. The absolute difference in baseline levels of FVIII:C and RCoF compared to third trimester levels in non-bleeders was statistically significant: FVIII:C (p=0.0001; absolute difference of 53.6 IU/dL), RCoF (p=0.0001; absolute difference of 65.7 IU/dL), respectively. There was no statistically significant rise in FVIII:C nor RCoF levels from baseline to third trimester in women who had bleeding events (Table 1).
Discussion:
A reasonable estimate for the rate of postpartum hemorrhage in the general population is 1-5%. Our study demonstrated a much higher rate of postpartum bleeding in patients with VWD with a higher rate of hemorrhage in C-sections than vaginal deliveries. In those patients selected for epidural administration of regional anesthesia there were no complications. It appears that the rise in factor VIII:C and RCoF levels from baseline predicted the absence of bleeding and a larger absolute increase of VIII:C and RCoF from baseline levels predicted the absence of postpartum bleeding. In patients with postpartum bleeding, there was a smaller absolute increase in factor VIII:C and RCoF. In both groups, there were bleeding events despite prophylactic treatment prior to delivery.
Conclusion:
Our study suggests that greater increases of factor VIII:C and RCoF from baseline may predict the absence of postpartum hemorrhage in patients with VWD. Larger studies are needed to further elucidate the relationship between factor VIII:C and RCoF levels at baseline and peripartum and the risk of postpartum hemorrhage.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal